Finally, expert neurology care at your fingertips
Neura Health is a comprehensive virtual neurology clinic. Meet with a neurology specialist via video appointment, and get treatment from home.

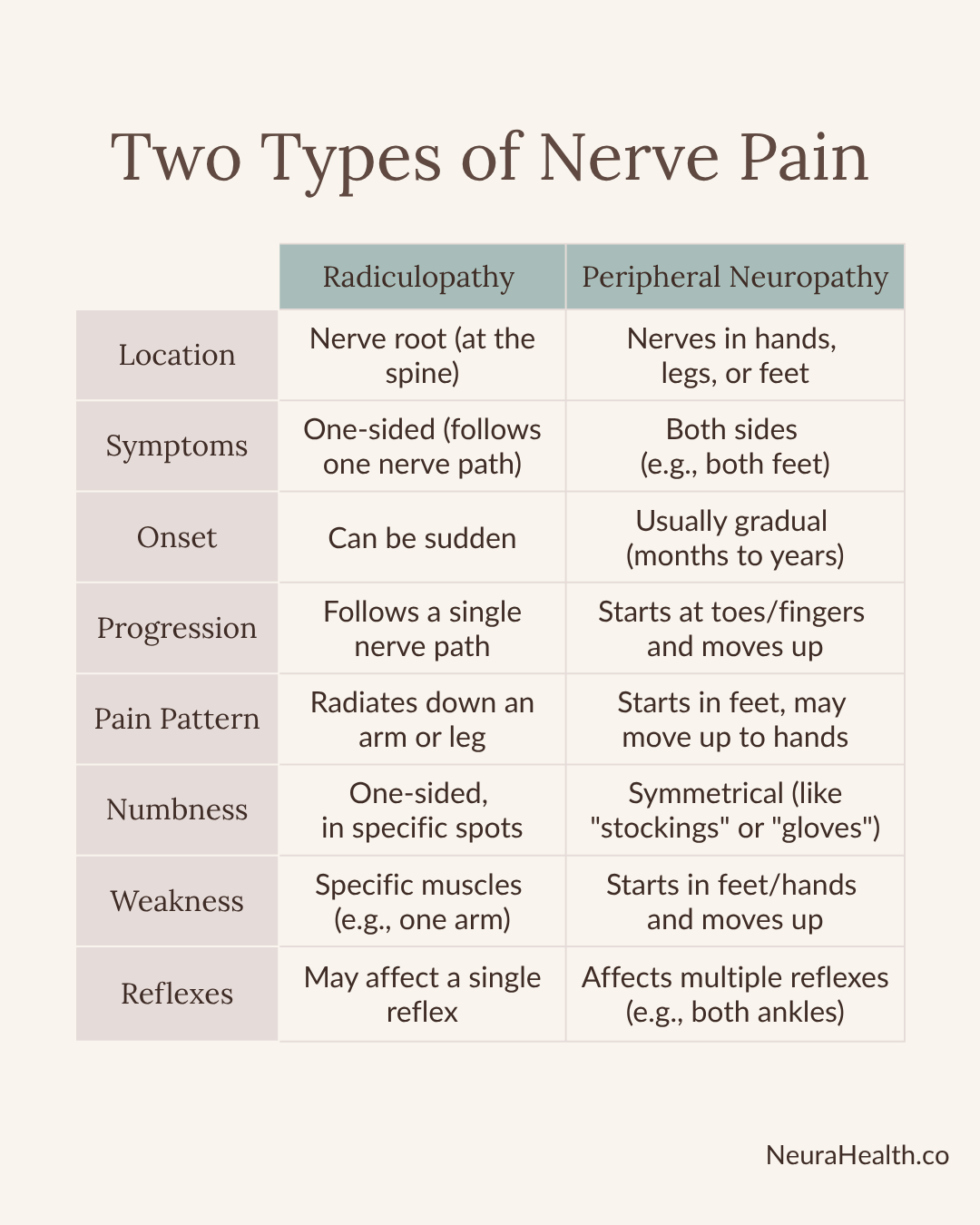
Nerve pain, also known as neuropathy, often presents as numbness, tingling, or pain in the arms or legs. But where is the pain coming from? While the symptoms feel similar, they can be caused by two very different problems:
Receiving the correct diagnosis is crucial because the treatments and outcomes vary significantly.
Radiculopathy is what most people call a "pinched nerve." It happens when a nerve root right at the spine is compressed or irritated. This could be due to spinal stenosis (narrowing of the nerve passageways), bone spurs from arthritis, or a herniated disk.
The signs of radiculopathy typically affect one side of the body and follow a specific path, known as a dermatome. Think of it as a "zone" that one specific nerve controls.
Peripheral neuropathy occurs when the more distal nerves (in your hands or feet) become damaged. The most common cause is diabetes, but it can also be caused by vitamin deficiencies (like B12, B1, or B6), kidney or liver disorders, thyroid disorders, heavy alcohol use, chemotherapy, or autoimmune conditions.
The most likely place for this compression is the wrist, otherwise known as Carpal Tunnel Syndrome. There are a few autoimmune conditions that also cause peripheral nerve damage, such as Guillain-Barre, CIDP, and Lupus. HIV, Lyme Disease, and HSV are a few of the viruses that can be toxic to peripheral nerves. And finally, a hereditary condition called Charcot-Marie-Tooth can cause congenital peripheral neuropathy.
If your doctor suspects radiculopathy, they may order an MRI of your spine. This test is excellent for seeing the cause, such as a herniated disk or spinal stenosis. A CT scan or X-ray might also be used.
If peripheral neuropathy is suspected, the first step is usually blood work, not imaging. These tests look for the cause, such as diabetes (A1C test), vitamin B12 deficiency, thyroid issues, or autoimmune markers.
If the diagnosis is still unclear, your neurologist may use a test called an EMG and NCS (nerve conduction study). This "gold standard" test measures the functioning of your nerves and muscles.
The goal is to relieve the pressure on the nerve. Fortunately, most cases improve without surgery.
Treatment focuses on addressing the underlying cause of the condition.
Regardless of the cause, you should go to the emergency room immediately if you experience any of the following:
If you're experiencing nerve-related symptoms, book a visit with one of our specialists at Neura Health. The sooner you understand what's happening, the sooner you can get the right treatment.
Neura Health is a comprehensive virtual neurology clinic. Meet with a neurology specialist via video appointment, and get treatment from home.
.png)