Finally, expert neurology care at your fingertips
Neura Health is a comprehensive virtual neurology clinic. Meet with a neurology specialist via video appointment, and get treatment from home.
Diagnosing neurological conditions often means looking closely at how your nervous system is built and how it functions. In many other areas of medicine, a physical exam can reveal many answers. But in neurology, specialized tests are often needed to see the brain, check its electrical signals, or find changes that can only be seen by looking inside the body.
The choice of which test to order depends on your specific symptoms and the clinical questions your neurologist still needs answered. These tests are sometimes an important piece of a puzzle that the neurologist has yet to fit together.
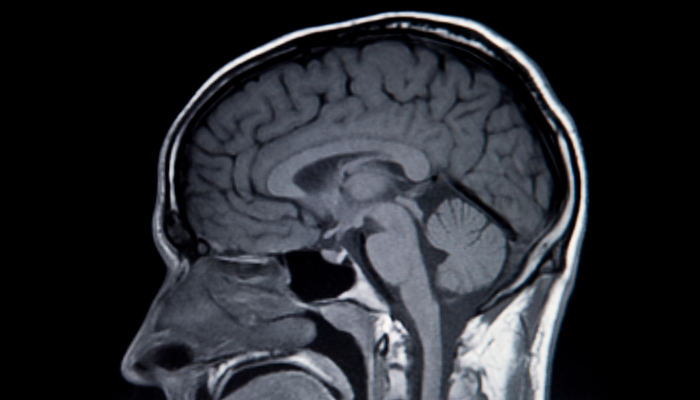
Each test has its own role in checking your nervous system. An MRI scan gives detailed images of soft tissues, while a CT scan is beneficial for looking at bones or sudden changes. An EEG records your brain’s electrical activity while it is happening.
There are many uses for different scenarios. A quick CT scan during an emergency, an MRI of the spine for chronic pain or weakness, or serial CTs to monitor the progress of a resolving brain hemorrhage are just a few examples of how neurologists would use these tests to help diagnose a condition.

What it shows: Detailed pictures of your brain and spinal cord, including soft tissues, blood vessels, and any abnormalities.
Why it's ordered: To look for stroke, tumors, different types of lesions, spine problems, or other structural abnormalities that might explain various symptoms like headaches, weakness, numbness, or cognitive changes.
What to expect: You'll lie on a table that slides into a large, tunnel-like machine. The test takes 30-60 minutes and is quite loud; you'll need to wear headphones or earplugs. The machine uses powerful magnets, so all metal objects must be removed.
The reality: Many people feel claustrophobic, but you can usually listen to music, and the technologist can talk to you throughout. Some facilities offer "open" MRIs, which are less confining.
Contrast dye: Occasionally, you may receive an injection that helps certain areas appear more clearly. This procedure is generally painless and very safe.

What it shows: Cross-sectional X-ray images that are used to visualize the brain and skull, bleeding (in the brain or on the scalp), and some brain abnormalities such as lesions or masses.
Why it's ordered: Often used in emergencies to quickly check for brain bleeds, skull fractures, or swelling. Also helpful for identifying sinus problems that may cause headaches. In most cases, it can be used to see new strokes, which is why it is used so often in the emergency room. It can also see some old strokes that have occurred in the past, as well as age-related vessel changes.
What to expect: You'll lie on a table that moves through a large, donut-shaped machine. The actual scan takes just a few minutes, although preparation and positioning may add an additional 10-15 minutes.
The reality: Much faster and less confining than MRI. The machine is quiet, and you can see out both ends of the scanner. Most people find CT scans much easier to tolerate.
Contrast dye: Sometimes used to highlight blood vessels or certain abnormalities. May be given by mouth, IV, or both.

What it shows: The electrical activity in your brain (essentially your brain waves).
Why it's ordered: Primarily to diagnose seizures or epilepsy; less commonly to evaluate confusion, memory problems, or consciousness disorders. It can help distinguish between seizures and other similar conditions.
What to expect: Small electrodes (like stickers) are placed on your scalp with paste or gel. You'll lie quietly while the machine records your brain's electrical activity for 20-60 minutes.
The reality: Completely painless, though the electrode paste can be a bit messy and takes some scrubbing to remove from your hair. You might be asked to breathe deeply, look at flashing lights, or try to fall asleep.
Special types: Occasionally, longer monitoring is necessary. You may wear a portable EEG at home for a specified period of time, or, in rare cases, stay in the hospital for several days of continuous video monitoring.
These tests excel at detecting structural changes and clear abnormalities. MRIs and CTs are particularly effective at identifying any abnormalities that alter the normal anatomy of your brain or spine. EEGs capture electrical abnormalities when they're actively occurring.
There are some neurological conditions that are functional rather than structural, meaning the anatomy is normal, and you are experiencing symptoms due to a non-neurologic cause. Additionally, some conditions are intermittent (they may not be active during the specific time window when you're being tested) and cannot be seen on a scan or EEG.
The timing of testing also plays a significant role. Some changes only become visible on scans after a certain amount of time has passed, while others might only be detectable in the acute phase of a condition.
Knowing these limits can help you understand why your doctor might suggest repeating tests later, or why normal results don’t always mean nothing is wrong. As previously mentioned, these tests are just one piece of the puzzle, and the rest of it - your history, symptoms, and exam - is also required to make it complete.
In neurology, providers often determine a diagnosis by first ruling out other causes. This might feel like overkill, but it’s actually a careful and effective way to get the right answer.
When your provider orders a test for symptoms that seem "obvious," they're following established diagnostic pathways that help ensure nothing serious is being missed. It is never a good thing to assume. Each person's diagnostic journey is tailored to their unique situation.
If your test results are normal, it doesn’t mean nothing is wrong. It just means the test that was ordered didn't find any abnormalities. Many common neurological conditions often have normal scans and test results.
Headache disorders, vestibular disorders, most movement disorders, and many types of seizure disorders typically don't show any significant abnormalities scans. Functional neurological conditions and early-stage neurodegenerative diseases often have normal initial testing as well.
Normal results are still helpful. They help your provider rule out serious problems and focus on what is more likely to be causing your symptoms. It focuses your care in a more productive way.
Sometimes neurologists order the same test again months or years later to re-evaluate a condition. Neurological conditions often evolve over time. For example, lesions due to multiple sclerosis are known to increase and/or decrease in size and quantity on repeat MRIs. Seizure activity may not be detected during a routine EEG, but could be captured during a longer study.
Repeat tests can show if your condition has changed or identify something that didn’t appear the first time.
Each test has specific strengths and blind spots.
Most tests are read by a radiologist (for MRI/CT) or neurophysiologist (for EEG) and then interpreted by your neurologist in the context of your symptoms and examination. If a CT was performed, and something was seen on the scan that the radiologist was unable to visualize clearly or appropriately, an MRI may be recommended as a next step.
You’ll usually get your results in a few days, unless it’s an emergency, in which case they’re reviewed right away. If you don’t hear back quickly, it often means nothing serious was found. If you feel too much time has passed, don't be afraid to reach out and ask about your results.
Before the test:
After the test:
At Neura Health, our specialists have a lot of experience with these tests and use them as part of your overall neurological care.
If you have questions about these tests or need a neurological check-up, we’re here to help. Book a visit with us anytime.
Neura Health is a comprehensive virtual neurology clinic. Meet with a neurology specialist via video appointment, and get treatment from home.
.png)